PBM FAQ
How pharmacy benefit managers hurt your health, your wallet, and your tax bill

PBMs Keep Manufacturer Rebates? Can They Do That?
PBMs work with drug makers to develop the list of medications to be covered by a given health plan. In the process PBMs negotiate, and are incentivized by, manufacturer rebates -- which they keep in part or whole. The more expensive the covered drug, the higher the rebate. And while the term “rebate” usually means the buyer receives some money back post-purchase, this is not the case for prescriptions. The patient buys the product but the PBM receives the rebate. PBMs will often structure their contracts to allow them to collect and keep rebates as part of an “administrative fees” or “rebate sharing” arrangement with the health plan instead of passing the rebate to its rightful owner - the purchaser of the prescription.
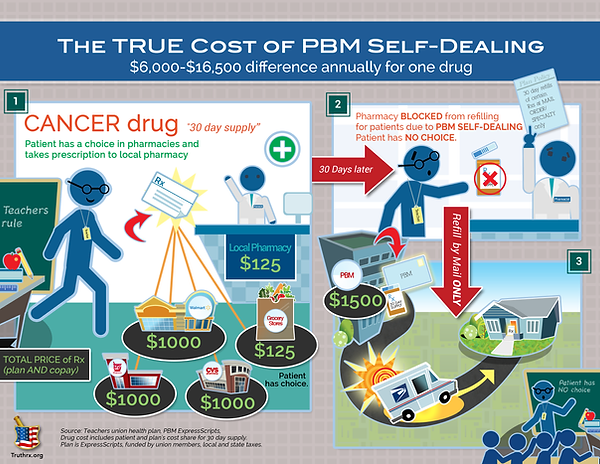
Why are PBMs Allowed to Own Pharmacies? Isn’t That a Conflict of Interest?
Currently there’s no law preventing PBMs from owning retail, mail order, specialty or any other type of pharmacy - a clear conflict of interest since PBMs not only negotiate which drugs will be covered and at what cost, they have direct and proprietary access to their prescription drug benefit plan enrollees and can use their access as a platform to guide, steer, direct or mandate which pharmacies plan enrollees can use. PBMs use their role as drug plan administrator to entice plan enrollees to use PBM pharmacies by offering incentives to patients that they directly disallow other pharmacies to use. For example, a PBM can offer a 90-day medication supply for the price of 60 days at its mail order pharmacy, but prohibits the local community pharmacy in your neighborhood from being able to do the same thing, even though your community pharmacy may be part of the PBM’s pharmacy network. Furthermore, CVS and Express Scripts have been caught in the act - and fined - for engaging in misleading scare tactics that pull patients away from their local pharmacies to a CVS or Express Scripts “preferred status” (large retail) pharmacy, claiming if patients don’t leave their local pharmacy, the price of their medication will greatly increase.

What’s a “Gag Clause” and How Do I Get Around It?
Though against the law nationally and in most states, “gag clauses” are contractual mandates that prevent your pharmacist from voluntarily disclosing if you would save money purchasing your medication directly instead of through your insurance plan. PBMs don’t want patients to know about better “cash” pricing and often include “gag clauses” in their contracts with pharmacies. Pharmacists who break the gag clause in their contracts are subject to serious financial penalties and so usually will not offer this information to the patient unless asked. The only way around the gag clause is for the patient to ask the pharmacist if they can get a better “cash” price on the prescription.
Why do Pharmacies Contract with PBMs?
But because pharmacies are dependent on having patients, and most patients depend on having a prescription drug plan to help offset the cost of expensive medications, pharmacies are left in a “take it or leave it” situation, business-wise. Most pharmacists take it, because they are in the business of providing care and the PBMs have the patients.
How Are Taxpayers Affected by PBMs?
Recent investigations in states like Ohio, Kentucky, Michigan, Mississippi, and Arkansas have uncovered serious questions about the level of profiteering PBMs that managed Medicaid may be engaged in. As with private health plans, PBMs provide a third-party prescription drug benefit plan to Medicaid and Medicare enrollees and bill the government for their services. State government pays for services with money raised by local taxes and receives matching federal funding (also taxes) to cover costs. In Ohio, an independent investigation by the Columbus Dispatch has shown CVS Caremark has been charging the state as much as 9 times the cost of a prescription drug while reimbursing local pharmacies below cost - meaning state taxpayers are paying CVS several times more than the going price for several common medications -- while CVS Caremark keeps the profits for themselves in a practice known as "spread pricing".
What is Spread Pricing?
Perhaps the most egregious of so-called PBM “proprietary” business tactics, spread pricing is the practice of charging the health plan payer several times more than the actual cost of the drug. While adding a mark-up to a good or service is standard business practice and not illegal, what makes this practice alarming is how PBMs have been shown to reimburse pharmacies at or often below (sometimes far below) the cost of the drug but then charge the health plan a price several times more than drug cost. The health plan administrators think they are paying the true cost of the drug while the local pharmacy hasn’t been paid enough to cover the cost of goods sold. The result is a fomenting crisis among smaller independent and community pharmacies that can no longer afford to keep their doors open or employ staff and are forced to close. The closure of small business pharmacies mostly affects communities and rural areas with populations of less than 50,000 and leaves patients with diminished access to medication while health plan sponsors and taxpayers are left to foot the much-higher bill.

How do they get away with it?
The lack of regulatory oversight and demand for transparency in the PBM industry has allowed PBMs to overcharge for prescription drugs for decades. PBMs typically don’t provide clients with complete, itemized billing statements so it’s only when informed patients and health plan sponsors “put 2 and 2 together” that they begin to understand how they’re probably greatly overpaying for their prescription medications while the “savings” they thought they would see go directly into the pockets of the PBMs - and their shareholders.
What can I do about it?
Several things. Talk to your local community pharmacist to understand how your drug plan influences the price you pay for medications. If you manage an employee benefit plan, ask your broker or PBM representative to provide a detailed explanation of your fee structure or contact PUTT for information on switching to a transparent “pass-through” PBM.
